This clinical simulation deals with tetanus, a
life-threatening infection. Tetanus is caused by an exotoxin synthesized by the
bacterium Clostridium tetani. The toxin is released after a wound is
infected by this bacterium. This toxin causes muscle spasm, which may lead to
death if not treated correctly. Spasms of the masseter (jaw) muscles have led to
the name lockjaw. Every time a patient with a wound is examined, the physician
must determine the appropriate immunization for the prevention of tetanus. This
simulation will help you understand the different approaches to the prevention
of tetanus as well as the indications for each approach. The immunologic
concepts addressed in this problem are fundamental to the understanding of many
other diseases.
When you have completed this activity you should be able to
1) define and give several examples of immunity.
2) compare and contrast the terms antigen and antibody.
3) differentiate between active and passive immunization
and be able to give examples of each.
4) compare and contrast the primary and secondary immune
responses in terms of their time course and magnitude.
5) state differences between adaptive (acquired) and
innate immunity, as well as between specific and non- specific immunity.
6) state which cell types are involved with cell-mediated
and antibody-mediated immunity.
7) compare tetanus toxin and tetanus toxoid relative
to toxicity and ability to cause an immune response.
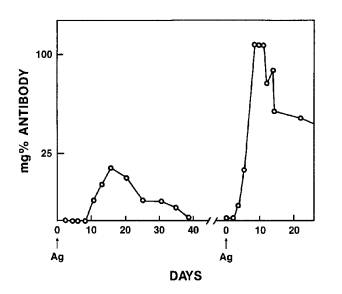
Question: Using the following graph, how many days does it take to
detect antibody in the serum after a primary and a secondary immunization,
respectively? The arrows above "Ag" refer to the times when antigen
injections were given to the patient. The term "mg% Antibody" refers
to the amount of antibody (in milligrams) detected in 100 ml of the patient's
serum.
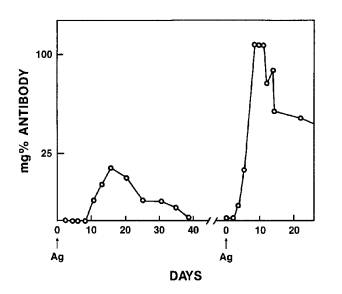
(A) 15 and 10
(B) 10 and 15
(C) 10 and 4
Instructions for the Clinical Problem
Each of the four group members has a different case history.
First, deal with your own patient. After reading your patient's case history,
decide the therapy you would use, the reasons for the choice, and the
consequences of alternative therapy. Next, fill out your answer sheet concerning
your patient. After everybody has finished his/her problem, the group member
with the first patient should present that case history to the other three group
members and allow them time to individually decide therapy, the reasons for
their choice, and the consequences of alternative therapy. They should then fill
out their answer sheets for that patient (i.e., commit themselves to therapy
before the group discussion). The group member who has the first patient should
then present his/her choice of therapy to the group and defend it. Members who
disagree with this choice, the reasons for it, or consequences of it should
present their ideas and defend them. After discussion of the first patient is
completed, compare your answers with those on the correct answer sheet for each
patient.
This process will then be repeated for the other three cases.
Patients should be presented in numerical order. At first glance, the patients'
cases seem repetitious, but there are subtle and important differences that
will help you decide how to treat the patient! These will be highlighted with
italics and bolding.
Remember, this is an "open-book" activity and you
should consult your textbooks about any point you don't understand.
First Patient: Joe Alsop
A 25 year old ex-serviceman arrives at your office with a
one-inch laceration (cut) of his right forearm caused by a dog bite through his
wool shirt. The dog, which belongs to a neighbor, has had rabies shots and is
chained so that he can be watched to be certain he doesn't have rabies. But your
real concern is possible infection, especially tetanus, since that is the most
immediate life-threatening consequence of the event. Joe tells you that he
received a tetanus vaccine when he joined the Army after graduating from high
school. On the therapy sheet, first decide which treatments would be
effective. Then decide which would be best, and write down your reasons for your
decision. Indicate your therapy on the "Joe Alsop" part of the Tetanus
Immunity Clinical Problem Answer Sheet (next page).
Clinical Problem Answer Sheet
Check the box(es) that indicate(s) the preferred therapy for
each patient. Then briefly write the reasons for your choice in the space
provided. Finally, describe the consequences of each of the other therapies in
the space provided under each therapy. Commit yourself in writing before the
discussion begins and have your group mates do the same. The answer sheet will not
be collected.
Joe Alsop (First Patient)
1. Give tetanus toxin.
2. Give tetanus toxoid.
3. Give tetanus antitoxin (horse).
4. Give tetanus immune globulin (human).
Kathleen Williams (Second Patient)
1. Give tetanus toxin.
2. Give tetanus toxoid.
3. Give tetanus antitoxin (horse).
4. Give tetanus immune globulin (human).
Tommy Criton (Third Patient)
1. Give tetanus toxin.
2. Give tetanus toxoid.
3. Give tetanus antitoxin (horse).
4. Give tetanus immune globulin (human).
Alice Wipple (Fourth Patient)
1. Give tetanus toxin.
2. Give tetanus toxoid.
3. Give tetanus antitoxin (horse).
4. Give tetanus immune globulin (human).
Instructions for the Clinical Problem – Student 2
The purpose of this exercise is to allow you to apply your
knowledge of active vs passive immunization and primary vs secondary
immune response to a common medical problem.
Each of the four group members has a different case history.
First, deal with your own patient. After reading your patient's case history,
decide the therapy you would use, the reasons for the choice, and the
consequences of alternative therapy. Next, fill out your answer sheet concerning
your patient. After everybody has finished his/her problem, the group member
with the first patient should present that case history to the other three group
members and allow them time to individually decide therapy, the reasons for
their choice, and the consequences of alternative therapy. They should then fill
out their answer sheets for that patient (i.e., commit themselves to therapy
before the group discussion). The group member who has the first patient should
then present his/her choice of therapy to the group and defend it. Members who
disagree with this choice, the reasons for it, or consequences of it should
present their ideas and defend them. After discussion of the first patient is
completed, compare your answers with those on the correct answer sheet for each
patient.
This process will then be repeated for the other three cases.
Patients should be presented in numerical order. At first glance, the patients'
cases seem repetitious, but there are subtle and important differences that
will help you decide how to treat the patient! These will be highlighted with
italics and bolding.
Remember, this is an "open-book" activity and you
should consult your textbooks about any point you don't understand.
Second Patient: Kathleen Williams
A 65-year-old woman has just come into your office with a
deep puncture wound in the calf of her leg caused by a pitchfork in a gardening
accident. She could not remember if she had previously been immunized to
tetanus. After treating the wound, what would you do to prevent tetanus?
On the therapy sheet, first decide which treatments would be effective. Then
decide which would be best, and write down your reasons for your decision.
Indicate your therapy on the "Kathleen Williams" part of the Tetanus
Immunity Clinical Problem Answer Sheet. (next page)
Instructions for the Clinical Problem – Student 3
The purpose of this exercise is to allow you to apply your
knowledge of active vs passive immunization and primary vs secondary
immune response to a common medical problem.
Each of the four group members has a different case history.
First, deal with your own patient. After reading your patient's case history,
decide the therapy you would use, the reasons for the choice, and the
consequences of alternative therapy. Next, fill out your answer sheet concerning
your patient. After everybody has finished his/her problem, the group member
with the first patient should present that case history to the other three group
members and allow them time to individually decide therapy, the reasons for
their choice, and the consequences of alternative therapy. They should then fill
out their answer sheets for that patient (i.e., commit themselves to therapy
before the group discussion). The group member who has the first patient should
then present his/her choice of therapy to the group and defend it. Members who
disagree with this choice, the reasons for it, or consequences of it should
present their ideas and defend them. After discussion of the first patient is
completed, compare your answers with those on the correct answer sheet for each
patient.
This process will then be repeated for the other three cases.
Patients should be presented in numerical order. At first glance, the patients'
cases seem repetitious, but there are subtle and important differences that
will help you decide how to treat the patient! These will be highlighted with
italics and bolding.
Remember, this is an "open-book" activity and you should consult
your textbooks about any point you don't understand
Third Patient: Tommy Criton
A 5-day-old baby has just been brought to your
office by his mother, a Peace Corps nurse. Mother and baby have just flown in
from Africa, where the baby was born. The mother is concerned because the baby
was cared for by a native friend. She discovered that the umbilicus (umbilical
cord) of the baby was coated with cow manure, a primitive local custom, and she
is concerned about neonatal tetanus. You find out that the mother was
vaccinated for tetanus when she joined the Peace Corps two years earlier.
What do you plan to do? On the therapy sheet, first decide which treatments
would be effective. Then decide which would be best, and write down your reasons
for your decision. Indicate your therapy on the "Tommy Criton" part of
the Tetanus Immunity Clinical Problem Answer Sheet. (next page)
Instructions for the Clinical Problem – Student 4
The purpose of this exercise is to allow you to apply your
knowledge of active vs passive immunization and primary vs secondary
immune response to a common medical problem.
Each of the four group members has a different case history.
First, deal with your own patient. After reading your patient's case history,
decide the therapy you would use, the reasons for the choice, and the
consequences of alternative therapy. Next, fill out your answer sheet concerning
your patient. After everybody has finished his/her problem, the group member
with the first patient should present that case history to the other three group
members and allow them time to individually decide therapy, the reasons for
their choice, and the consequences of alternative therapy. They should then fill
out their answer sheets for that patient (i.e., commit themselves to therapy
before the group discussion). The group member who has the first patient should
then present his/her choice of therapy to the group and defend it. Members who
disagree with this choice, the reasons for it, or consequences of it should
present their ideas to the group and defend them. After discussion of the first
patient is completed, compare your answers with those on the correct answer
sheet for this patient.
This process will then be repeated for the other three cases.
Patients should be presented in numerical order. At first glance, the patients'
cases seem repetitious, but there are subtle and important differences that
will help you decide how to treat the patient! These will be highlighted with
italics and bolding.
Remember, this is an "open-book" activity and you
should consult your textbooks about any point you don't understand.
Fourth Patient: Alice Wipple
A 35-year-old migrant worker arrives at your office with a
three-inch jagged wound on her head. She was hit with a brick. Ten years ago she
fell off a tractor while tilling a field and received a six-inch laceration
(cut) of her left thigh. At that time, she was given tetanus antitoxin
from a horse because she had never been immunized against tetanus. But she and
her fellow migrant workers left town before her physician could immunize her
with tetanus toxoid. What do you do to prevent tetanus? On the therapy
sheet, first decide which treatments would be effective. Then decide which would
be best, and write down your reasons for your decision. Indicate your therapy on
"Alice Whipple" part of the Tetanus Immunity Clinical Problem Answer
Sheet.
Clinical Problem Answer Sheet
Check the box(es) that indicate(s) the preferred therapy for all
patients. Then briefly write the reasons for your choice in the space
provided. Finally, describe the consequences of each of the other therapies in
the space provided under each therapy. Commit yourself in writing before the
discussion begins. The answer sheet will not be collected.
Joe Alsop (First Patient)
1. Give tetanus toxin.
2. Give tetanus toxoid.
3. Give tetanus antitoxin (horse).
4. Give tetanus immune globulin (human).
Kathleen Williams (Second Patient)
1. Give tetanus toxin.
2. Give tetanus toxoid.
3. Give tetanus antitoxin (horse).
4. Give tetanus immune globulin (human).
Tommy Criton (Third Patient)
1. Give tetanus toxin.
2. Give tetanus toxoid.
3. Give tetanus antitoxin (horse).
4. Give tetanus immune globulin (human).
Alice Wipple (Fourth Patient)
1. Give tetanus toxin.
2. Give tetanus toxoid.
3. Give tetanus antitoxin (horse).
4. Give tetanus immune globulin (human).
Congratulations, you have finished the clinical problems! Now
you should answer these posttest questions below, individually. After you’ve
completed them, check your answers against the posttest answer sheet.
Posttest –
Instructions: Please mark your answers to the following
questions on this sheet. Choose the one correct or best answer.
1. A 23 year old medical student had four injections of
diphtheria, pertussis, and tetanus (DPT) in her first year of life and a booster
at age 5, but no booster for tetanus after that. She was bitten by a mouse while
doing an experiment. She should be given
-
(A) tetanus toxoid, which will passively immunize her.
-
(B) tetanus antiserum (human), which will passively immunize
her.
-
(C) tetanus toxoid, which will actively immunize her.
-
(D) tetanus antiserum (human), which will stimulate a memory
response.
2. A 10-year-old girl who received a deep cut